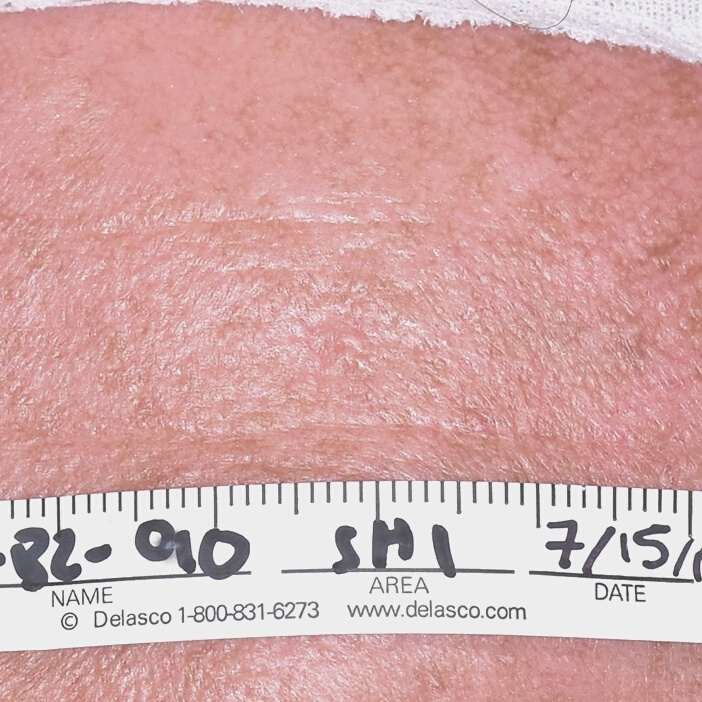
In this video Dr. Nakatsui is removing two sebaceous cysts located on the scalp. Our lovely patient graciously allowed us to film the procedure and we thank you for that!
In this video the two cysts come out relatively easily and intact as a whole. There will be several instances where we are not so lucky and the cyst may fragment or it may adhere to surrounding tissue more making extraction more difficult.
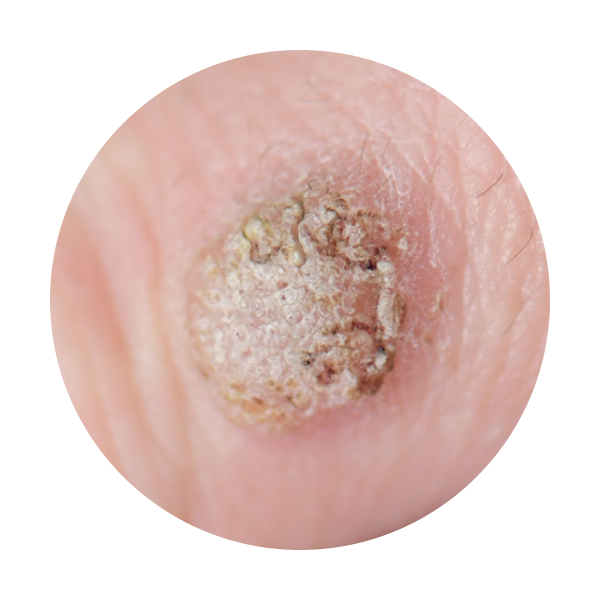
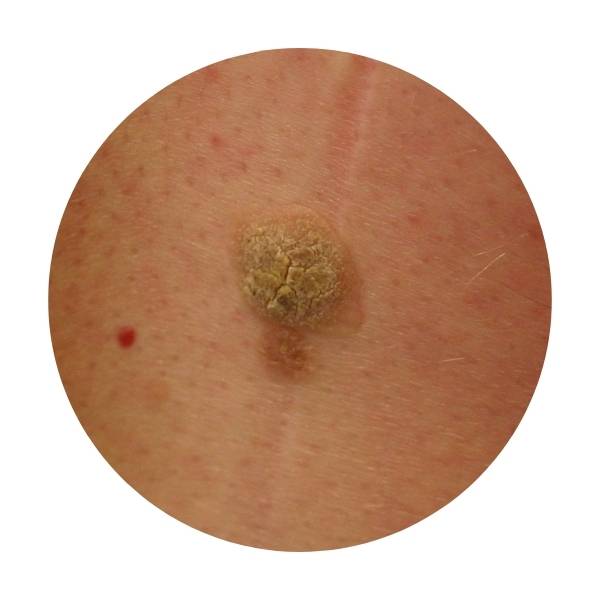
Sebaceous cysts may occur anywhere on the body at any time of our lives. They are generally not life-threatening, but when concerned about any lesion, it is always best to seek medical attention. Many patients with sebaceous cysts may leave them as they generally will not bother them. From time to time, cysts may become inflamed, painful, produce discharge, or become infected. If a cyst has had repeated infection/inflammation or self attempts to extract the contents by squeezing the cyst, this is when the cyst wall may become more adherent to surrounding tissue making it difficult to extract.
Should a cyst develop, it is advisable not to perform self surgery as any tools used to puncture the skin or extract the cyst may push unwanted bacteria into the site causing an infection. Not only that, if the wound site is not properly closed or should become infected, when it fully heals you may be left with an unwanted scar which may be difficult to treat in the future.